Subscribe to our Newsletter
Receive our weekly newsletter, updates, and promotions, to your inbox.
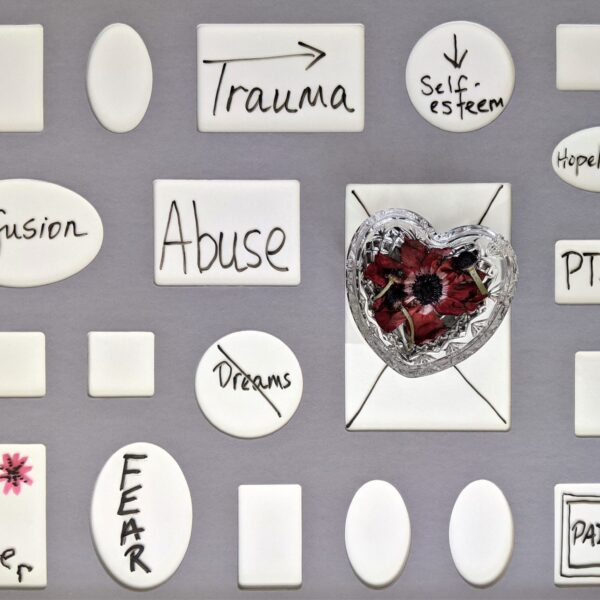
There is increasing recognition that autism and trauma are associated in significant ways which contribute to our understanding of autism, our awareness of the importance of the assessment of trauma in the diagnostic assessment process, and the types of support and treatment offered.
Our current diagnostic manual, DSM5-TR defines trauma as “actual or threatened death, serious injury, or sexual violence” (APA, 2022, page 301). To be diagnosed with Post-Traumatic Stress Disorder (PTSD) using the DSM5, the person must have experienced this type of trauma, and demonstrate trauma symptoms with functional impairment including:
persistent re-experiencing of the event, via flashbacks and/or nightmares and/or involuntary distressing memories of the trauma;
avoidance of internal and/or external thoughts or reminders about the trauma;
signs of worsening cognition or mood after the trauma for eg, persistent and exaggerated negative beliefs about oneself, others and the world; inability to experience positive emotions;
Changes in reactivity and arousal after the trauma, for eg, hypervigilance, sleep disturbance, problems with concentration.
However, it is possible to experience different types of trauma and still show the symptoms of PTSD. For example, children who experience high levels of exposure to neighbourhood violence, parental divorce, traumatic loss, poverty, mental illness, and substance abuse in the family (adverse childhood experiences or ACEs) may develop PTSD symptoms and meet criteria for Complex-PTSD (trauma symptoms in reaction to a series of traumatic events over time). These children have been found to be at higher risk for poorer medical, psychiatric, and socioeconomic outcomes across their lifetimes (Felitti, et al 1998). The higher number of ACEs they experience, the higher their risk of poor outcomes across multiple dimensions.
There is a growing recognition that autistic people are at higher risk of experiencing traumatic events. For example, Berg and colleagues (2016) in a population-based study found a significantly higher proportion of adverse childhood experiences (ACEs) for autistic children compared to nonautistic children. People with developmental disabilities, including autism and intellectual disability, have been found to be three times more likely to experience trauma compared to their typically developing peers (Hibbard and Desch, 2007; Reiter et al; 2007). Kerns et al (2017) also found that the risk of trauma for autistic children was greater in lower income families.
Two studies (Griffiths et al, 2019; Rumball, 2019) found that autistic adults are significantly more likely than their same-aged peers to experience adverse events leading to PTSD and other mental health conditions. The most common adverse events were loss of study and work, and bullying.
For autistic people traumatic and adverse events do not automatically lead to PTSD but have been found to be associated with anxiety disorders and depression. Taylor and Gotham (2016) found that 90% of autistic adolescents with depression had experienced at least one trauma, compared to 40% of nondepressed autistic adolescents.
There is considerable research showing that early life stressors cause brain change, especially during critical periods of brain development (Agorastos et al, 2019). In their extensive review Teicher and colleagues (2016) conclude that early life stressors, in particular childhood maltreatment, are associated with significant brain change in adults, particularly in the hippocampus, corpus callosum, insula, dorsolateral prefrontal cortex (PFC), orbitofrontal cortex, anterior cingulate gyrus, and caudate nucleus. Each of these areas has been implicated in the brain difference we see in autism.
Functional connectivity of the amygdala and PFC have been found in both autistic children and traumatised children (Mazefsky et al, 2013) leading some researchers to speculate that this neurological difference in autistic children may be due to early life stressors or the effects of chronic stress (Rudie, et al, 2012; Liu et al, 2020).
Regardless of the cause of the differences in neurology, the result of is reduced capacity to self-regulate using taught strategies, and therefore the likelihood of experiencing periods of prolonged stress. The PFC is involved in the social and cognitive appraisal of a stressful situation, leading to the likelihood of experiencing even benign social interactions as being threatening, which commonly occurs for autistic adolescents and adults. In other words, trauma and prolonged stress cause neurological changes that mimic autism and cause further emotional disturbance and dysregulation.
We have discussed that autistic people are at higher risk of experiencing early life stressors and trauma and that these events may cause or exacerbate different brain functioning leading to both emotion regulation problems and long periods on ongoing stress, in a self-perpetuating cycle. It has also been recognised that some of the thinking and coping styles of being autistic can increase the risk of developing a trauma-related disorder, such as PTSD, c-PTSD or an attachment disorder.
For example, an autistic person is more likely to experience elevated baseline levels of anxiety due to social and sensory overload. Sensory overload is caused by a different sensory processing system where certain everyday sensory experiences cause pain, hypervigilance and difficulty concentrating. Social overload is caused by social confusion due to problems with ‘theory of mind’ (perspective-taking), being misunderstood, criticised or rejected by peers, and a tendency to misinterpret benign social experiences as being threatening.
Autism is associated with a cognitive style called ‘weak central coherence’ which is a tendency to focus on details at the expense of missing the “big picture.” We have found that clinically this can lead to an over-focus on certain negative aspects of life, whilst missing the parts of life that are going well. For example, a belief that one is a failure because of making a single mistake, whilst ignoring all the times they were successful. Unhelpful cognitive appraisal styles such an the one described, but also black-and-white thinking, (for eg, “he made a mean face therefore he is a mean person”) and catastrophising (for eg, able to jump to the worst possible conclusion in a nano-second), are common in autism, and are implicated in the development of stress and trauma-related disorders.
Other risk factors that are common to both autism and the development of a stress-related disorder include social withdrawal and isolation, a tendency to suppress and avoid difficult emotions, poor sleep, anxiety, and depression.
It is important for clinicians to be aware that clients presenting for a diagnostic assessment for autism may well have been subject to traumatic events. One condition can be missed due to diagnostic overshadowing. Assessing for whether trauma has occurred will inform both differential diagnoses, i.e. whether the person is autistic, traumatised or both, and what support and therapy to offer. The psychological effects of trauma do not vanish by themselves, but are treatable, and if the person is also autistic, treatment will need to be modified accordingly.
Being aware that your autistic client or loved one is at high risk for adverse life events including trauma, and more likely to develop a stress-related disorder as a result, provides a helpful pathway forward. Firstly, being protective is a key component. We cannot wrap the autistic person in cotton wool, but we can supervise, monitor, and shield as much as possible, especially if the autistic person in non-speaking or has an intellectual disability.
Secondly, we can be aware that an autistic child or adolescent tends to experience the world as being more threatening due to their social communication difficulties and a different sensory system. There are many accommodations we can make to ease their background anxiety, across home, school, and community settings, especially with a vigilant commitment to stop school and workplace bullying. Understanding autism, and seeing the world through their eyes, will give you insights in how to scaffold and accommodate your loved one or client, including informing your expectations of what and how much they can cope with.
Since many of the risk factors for developing a stress-related disorder are known, we can provide our autistic children and adolescents with the tools to read social situations with more accuracy, teach adaptive ways to appraise situations, and other tools for emotion regulation. We can scaffold and assist them to build friendships to inoculate them against social withdrawal and isolation. We can help them foster a strong sense of identity and resilience in the face of adversity by seeing, believing and fostering their strengths, abilities and passions.
Lastly, we can be aware of how to differentiate the effects of trauma from the expression of autism, so that we can offer access to psychological treatment to resolve trauma-related psychological issues. There is an emerging and much-needed literature on treatment adaptations for treating trauma-related disorders in autistic people, see for example, the review by Jessica Peterson and colleagues from the University of Washington, Seattle (2019), with particular guidelines related to trauma-focussed cognitive behaviour therapy (TF-CBT. There is also good preliminary evidence for the use of Eye Movement Desensitisation and Reprocessing (EMDR) therapy for autistic traumatised adults (Lobregt-van Buuren, et al 2018).
If you are a clinician interested in enhancing your discipline-specific skills in the diagnostic assessment of autism in children and adolescents, including teasing out differential and co-occurring conditions such as trauma-related disorders, we recommend our online course Masterclass 1: Diagnosis for Autistic Children and Adolescents.
We also focussed on providing support and therapy for autistic children and adolescents including many of the goals mentioned above, e.g. teaching tools to read social situations with more accuracy, adaptive ways to appraise situations, and tools for emotion regulation. This component of the course is suitable for professionals and parents seeking further ways to support their autistic child or adolescent.
Agorastos A., Pervanidou P., Chrousos G. P., Baker D. G. (2019b). Developmental trajectories of early life stress and trauma: a narrative review on neurobiological aspects beyond stress system dysregulation. Front. Psychiatry 10:118. 10.3389/fpsyt.2019.00118
APA, (2022). Diagnostic and Statistical Manual of Mental Disorders 5th edition Text Revision (DSM-5-TR), USA: American Psychiatric Association.
Berg KL, Shiu CS, Acharya K, Stolbach BC, Msall ME. (2016). Disparities in adversity among children with autism spectrum disorder: a population-based study. Developmental Medicine & Child Neurology; 58(11):1124–1131. doi 10.1111/dmcn.13161 https://doi.org/10.1111/dmcn.13161
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine. 1998;14(4):245–258.
Griffiths S, Allison C, Kenny R, Holt R, Smith P, Baron-Cohen S. )2019). The Vulnerability Experiences Quotient (VEQ): A study of vulnerability, mental health and life satisfaction in autistic adults. Autism Res; (12):1516–1528. https://doi.org/10.1002/aur.2162
Hibbard RA, Desch LW. Maltreatment of children with disabilities. Pediatrics. 2007;119(5):1018–1025.
Kerns CM, Newschaffer CJ, Berkowitz SJ, Lee BK. (2017). Examining the association of autism and adverse childhood experiences in the national survey of children’s health: The important role events of income and co-occurring mental health conditions. Journal of Autism and Developmental Disorders; 47:2275–2281. doi: 10.1007/s10803-015-2392-y https://doi.org/10.1007/s10803-015-2392-y
Kildahl AN, Bakken TL, Iversen TE, Helverschou SB. (2019). Identification of post-traumatic stress disorder in individuals with autism spectrum disorder and intellectual disability: A systematic review. Journal of Mental Health Research in Intellectual Disabilities;12:1–2. doi.org/10.1080/19315864.2019. 1595233 https://doi.org/10.1080/19315864.2019.1595233
Liu W. Z., Zhang W. H., Zheng Z. H., Zou J. X., Liu X. X., Huang S. H., et al. (2020). Identification of a prefrontal cortex-to-amygdala pathway for chronic stress-induced anxiety. Nat. Commun. 11:2221. 10.1038/s41467-020-15920-7
Lobregt-van Buuren E, Sizoo B, Mevissen L, de Jongh A. (2019). Eye Movement Desensitization and Reprocessing (EMDR) Therapy as a Feasible and Potential Effective Treatment for Adults with Autism Spectrum Disorder (ASD) and a History of Adverse Events. J Autism Dev Disord;49(1):151-164. doi: 10.1007/s10803-018-3687-6. PMID: 30047096.
Mazefsky, C. A., Herrington, J., Siegel, M., Scarpa, A., Maddox, B. B., Scahill, L., & White, S. W. (2013). The role of emotion regulation in autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 679–688. doi:10.1016/j.jaac.2013.05.006.
Peterson JL, Earl R, Fox EA, Ma R, Haidar G, Pepper M, Berliner L, Wallace A, Bernier R. (2019). Trauma and Autism Spectrum Disorder: Review, Proposed Treatment Adaptations and Future Directions. J Child Adolesc Trauma;12(4):529-547. doi: 10.1007/s40653-019-00253-5. Epub 2019 Apr 10. PMID: 31819782; PMCID: PMC6901292.
Reiter S, Bryen DN, Shachar I. (2007). Adolescents with intellectual disabilities as victims of abuse. Journal of Intellectual Disabilities;11(4):371–387.
Rudie J. D., Shehzad Z., Hernandez L. M., Colich N. L., Bookheimer S. Y., Iacoboni M., et al. (2012). Reduced functional integration and segregation of distributed neural systems underlying social and emotional information processing in Autism Spectrum Disorders. Cereb. Cortex 22, 1025–1037. 10.1093/cercor/bhr171
Rumball F. (2019) A systematic review of the assessment and treatment of post-traumatic stress disorder in individuals with autism spectrum disorders. Rev J Autism Dev Disord. (6):294–324. https://doi. org/10.1007/s40489-018-0133-9
Taylor JL , Gotham KO. (2016). Cumulative life events, traumatic experiences, and psychiatric symptomatology in transition-aged youth with autism spectrum disorder. Journal of developmental disorders ;8:28. doi 10.1186/s11689-016-9160-y https://doi.org/10.1186/s11689-016-9160-y
Teicher M. H., Samson J. A., Anderson C. M., Ohashi K. (2016). The effects of childhood maltreatment on brain structure, function and connectivity. Nat. Rev. Neurosci. 17, 652–666. 10.1038/nrn.2016.111